Dean's Update
November 22, 2024 - Aron Sousa, MD
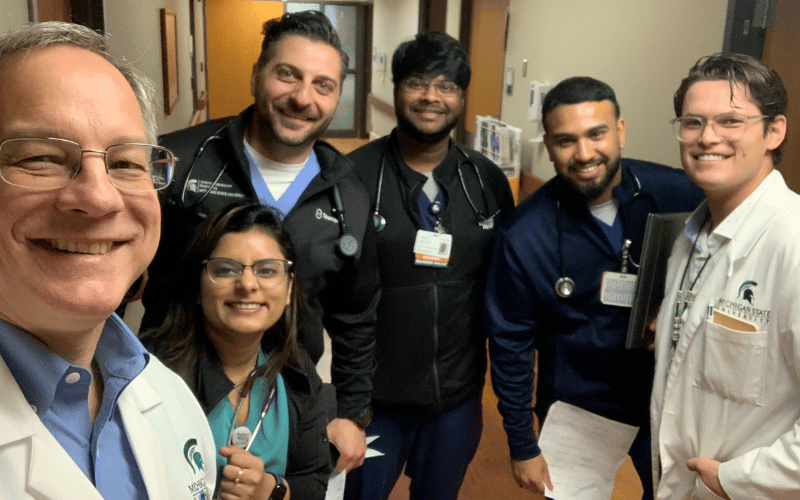
(Above) L-R, Aron on rounds with internal medicine residents, Drs. FNU Parul, PGY-1, Harith Ghnaima, PGY-3, Lalitsiri Atti, PGY-2, Nasatya Khadka, PGY-1, and third-year CHM student Hayden Wood.
Friends,
I am back on the Michigan State University internal medicine service. Regardless of what swirls around me, I really enjoy my two weeks with our students and residents on service. We take care of remarkably sick people from the Lansing area. In truth, I prefer working with sick patients and their families. The medicine is intense, the emotional work is clear, and it is easy to prioritize and focus on the next steps. None of that is true of being dean – rounding is a nice break from the rest of my job. But, without the residents it would not be possible for me to round, and this is a great team. I’ve worked with both Harith and Lalit before, and they are both excellent senior residents. Our first years are doing a great job with the patients, and Hayden, our intrepid medical student, is all in on the service and doing beautifully.
I am only a few days into my fortnight of rounding, but I have already been reminded of a particularly clever bit of evolutionary biology. During teaching rounds early in the week, Dr. Atti did an excellent presentation of a case of Serratia marcescens endocarditis. Serratia is in a group of bacteria that have inducible resistance to beta-lactam antibiotics, which include the penicillins and cephalosporins but also the carbapenems, for those of you who were wondering. If you culture and grow these bacteria from an untreated patient and test which antibiotics work against them, the bacteria will initially appear to be sensitive to beta-lactam antibiotics. But once you begin treatment with the beta-lactam antibiotic, a “switch” in the DNA of the bacteria is thrown, and the bacteria begin producing a beta-lactamase, an enzyme that destroys beta-lactams. With the initial culture, it looked like you had the right antibiotic to treat the patient’s infection, but if you culture and test the susceptibility of these bacteria after you start treatment with a beta-lactam, the bacteria will now be resistant to your beta-lactam antibiotic. Oh, and bacteria can trade these resistance genes between species of bacteria with little circles of DNA called plasmids. This is not a good turn for we humans, but it shows just how amazing evolution is. Diabolical for people but a cool bit of biology.
MSU Foundation associate professor Shannon Manning, PhD, and her team in the Department of Microbiology, Genetics, and Immunology, study antibiotic resistance and its evolution. In particular they study the bacteria and phages (viruses that infect bacteria) of our gut and the guts of animals. The microbiomes of the humans and animals are a major location of bacterial evolution, including the evolution of antibiotic resistance.
Care to avoid the worst of biology and the rest of the world? Giving Tuesday is December 3, and we are focused on the Spartan Cornerstone Challenge Endowed Scholarship and the MPH Student Support and Professional Development fund. Giving to the college will not help you avoid Serratia or the Helvetica Scenario, but our students are wonderful and need your support. This is a great opportunity for you to have a direct impact on the next generation of doctors and public health professionals who make a significant mark on communities. The college’s primary fundraising priority is student scholarships, and this helps address the struggle of student debt. Thanks for helping our students.
Serving the people with you,
Aron
Aron Sousa, MD, FACP
Dean, Michigan State University College of Human Medicine

