Progress Assessment Across the Curriculum
Student progress through the Shared Discovery Curriculum is based upon attainment of the knowledge, skills, and attitudes described within the Chief Complaints and Concerns (C3) documents and encompassed within the SCRIPT competencies. Students are assessed extensively throughout the Shared Discovery Curriculum through a longitudinal competency assessment using the Progress Suite of Assessments. From the first weeks of medical school, and at regular intervals throughout the curriculum, a suite of progress assessments enables students and their faculty to verify the achievement of competence and readiness to move through the curriculum.
Progress testing is a longitudinal competency assessment that facilitates adult learning. In essence, the College of Human Medicine Progress Suite of Assessments is the graduation test for the MD degree, measuring the entire body of knowledge that a student should master by the end of medical school. Rather than aiming for mastery of a small amount of knowledge, progress testing assesses incremental improvement in student performance over an extended period of time.
For both the Progress Clinical Skills Examination (PCSE) and Comprehensive Necessary Science Exam (CNSE), exams of comparable content and complexity are administered twice each semester. Students are expected to demonstrate incremental improvements and attain minimum levels of performance by the end of each semester for promotion to higher-level courses. Students receive reports of their performance on these exams at mid-semester and end of semester from the Office of Assessment. The Student Competence Committee considers the semester’s best performance for each component of the exams at its meetings. (For example, if the student performs at a higher level for mid-semester CNSE than the end of semester CNSE, the Student Competence Committee uses the mid-semester score.)
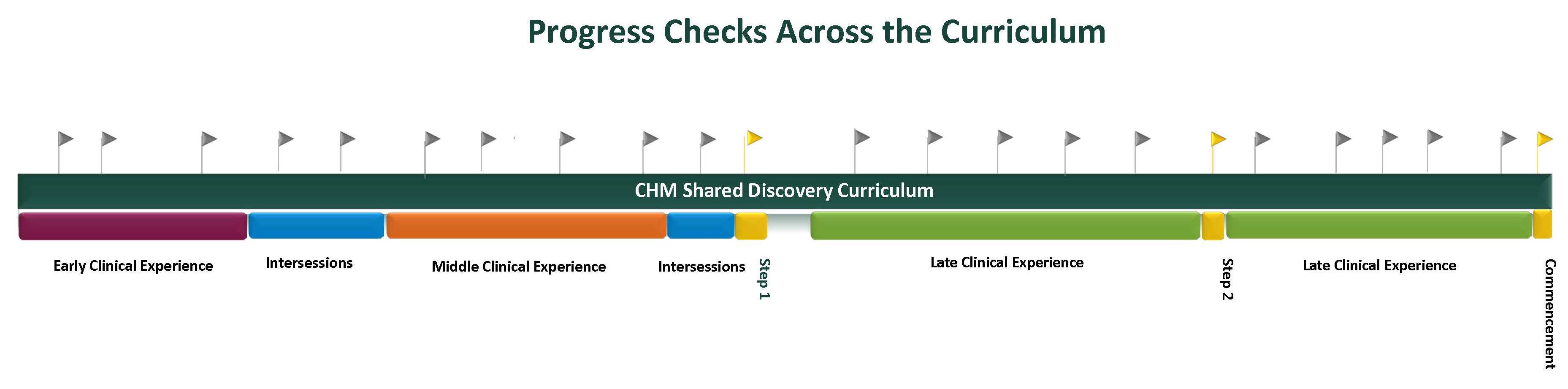
Progress suite assessments are offered twice a semester and are available to students of all levels of the curriculum. Students must pass the Progress Suite of Assessments in order to move through the curriculum. The combination of progress testing and experience-based education fuels individual learning planning so that every student can achieve their full potential.
The Progress Suite of Assessments
This summative group of assessments is comprised of six core components:
-
The Progress Clinical Skills Examination (PCSE) combines interactions with standardized patients and/or health professionals, use of manikins, clinical reasoning exercises, and clinical documentation in a simulation center within eight stations. Each station includes assessments of the knowledge, skills, or attitudes pertinent to learners across the spectrum of the curriculum including interactional skills, hypothesis-driven history gathering, hypothesis-driven physical examination, counseling skills, safety behaviors, clinical reasoning, and application of necessary science. Students spend 20 minutes at each station in an encounter with a standardized patient and then ten minutes answering related clinical and necessary science questions.
- The Comprehensive Necessary Science Examination (CNSE) utilizes electronic, multiple choice questions similar to Step 1 and Step 2 Clinical Knowledge United States Medical Licensing Examinations.
-
Multisource Feedback encompasses assessments from preceptors (clinical and non-clinical settings), peers (clinical and non-clinical settings), nurses, other health care team members, and patients.
-
The Portfolio is an aggregation of materials or artifacts that demonstrate the ongoing participation and development of the student. All artifacts and assessments within the Portfolio align with SCRIPT competency goals. Some of the materials/artifacts are generated by participation in activities or completion of assignments based on the curricular component and topic. Portfolios of evidence containing essays, videos, reflections, scholarly products and projects are reviewed at regular intervals by Learning Society Fellows. These reviews assure acquisition of the necessary knowledge, skills and attitudes, and that learners receive anticipatory guidance to achieve not only competence, but excellence. Examples include:
- Direct Observation: Preceptors observe students performing a variety of clinical skills, including but not limited to eliciting a history, performing a physical examination, counseling a patient, and giving an oral case presentation. The preceptor assesses student performance using pre-established assessment tools in Just In Time Medicine.
- Clinical Documentation: Students complete clinical documentation, such as History and Physical Exam documents, progress notes, discharge summaries, prescriptions, and post-encounter summaries, in real and simulated clinical settings. Each document is assessed using a pre-established rubric available within Just In Time Medicine.
- Logbooks: Students maintain procedure logbooks in Just In Time Medicine. Supervising personnel complete check off lists and global assessments of competence. The number and types of procedures required are described in curricular materials.
- Skill Certification: Opportunities to obtain specialized knowledge and skills pertinent to medical training exist outside of the College. Two are required:
- Current Basic Life Support (BLS) certification by the American Heart Association is required at the time of matriculation and must be maintained throughout enrollment.
- Michigan State University Institutional Review Board certification for researchers is required prior to graduation and any participantion in any human subjects research.
- Direct Observation: Preceptors observe students performing a variety of clinical skills, including but not limited to eliciting a history, performing a physical examination, counseling a patient, and giving an oral case presentation. The preceptor assesses student performance using pre-established assessment tools in Just In Time Medicine.
-
- External Examinations: Students must pass USMLE Step 1 to enter the LCE, and pass Step 2 Clinical Knowledge and Step 2 Clinical Skills to progress through the curriculum and be eligible for graduation. Additional information regarding these examinations is available at usmle.org.
- Formative Assessments: As students participate in laboratory, simulation,individual and team-based learning activities, a variety of formative assessments are generated. Students may choose to include some or all of these in their portfolios for review by the Student Competence Committee.
- Activities supporting Academic Certificate achievement: Students accepted to special programs within the medical school may earn academic Certificates (e.g. Rural Health Certificate) through completion of coursework or activities as specified in separate curricular documents. These activities and/or academic products may also be used as evidence of achievement of the SCRIPT competency goals.
- Additional artifacts: Additional materials require student selection, completion, and upload into Just In Time Medicine or other course management programs. Examples of these include reflective journals as part of the service project or quality improvement project reports and other artifacts chosen by the student to demonstrate competence.
- External Examinations: Students must pass USMLE Step 1 to enter the LCE, and pass Step 2 Clinical Knowledge and Step 2 Clinical Skills to progress through the curriculum and be eligible for graduation. Additional information regarding these examinations is available at usmle.org.
-
End of Semester Self-Assessments (ESSA) are part of the student's academic record and are reviewed by the Student Competency Committee. Students populate a SCRIPT-aligned rubric referencing assessments and portions of the portfolio as evidence of attainment of competency, and identifying personal learning goals for the following semester.
-
Individual Learning Plans (ILP) Students reflect upon formative and summative assessments on an on-going basis to create and maintain Individual Learning Plans that address areas of strength, areas for improvement, goals, and resources to help attain the goals. These are real-time, formative documents. Students review their ILPs with their assigned Learning Society Fellows on a regular basis. This includes mid-course feedback for students. The Fellows provide formative feedback to the student and an assessment of students’ engagement in the ILP process with the Student Competence Committee. (The ILP itself is not part of the academic record and is not reviewed by the Student Competence Committee.)

