NIH-Funded MSU Study Delivers Results in Rural Michigan
November 19, 2025
For a decade, Jane Hiske lived in denial of her diabetes diagnosis.
“I watched my own brother start out with just a sore on his foot. He had to have part of his foot taken off. Then the toes had to come off with another surgery. They ended up taking him at the knee. That’s when it hit me, this is serious."
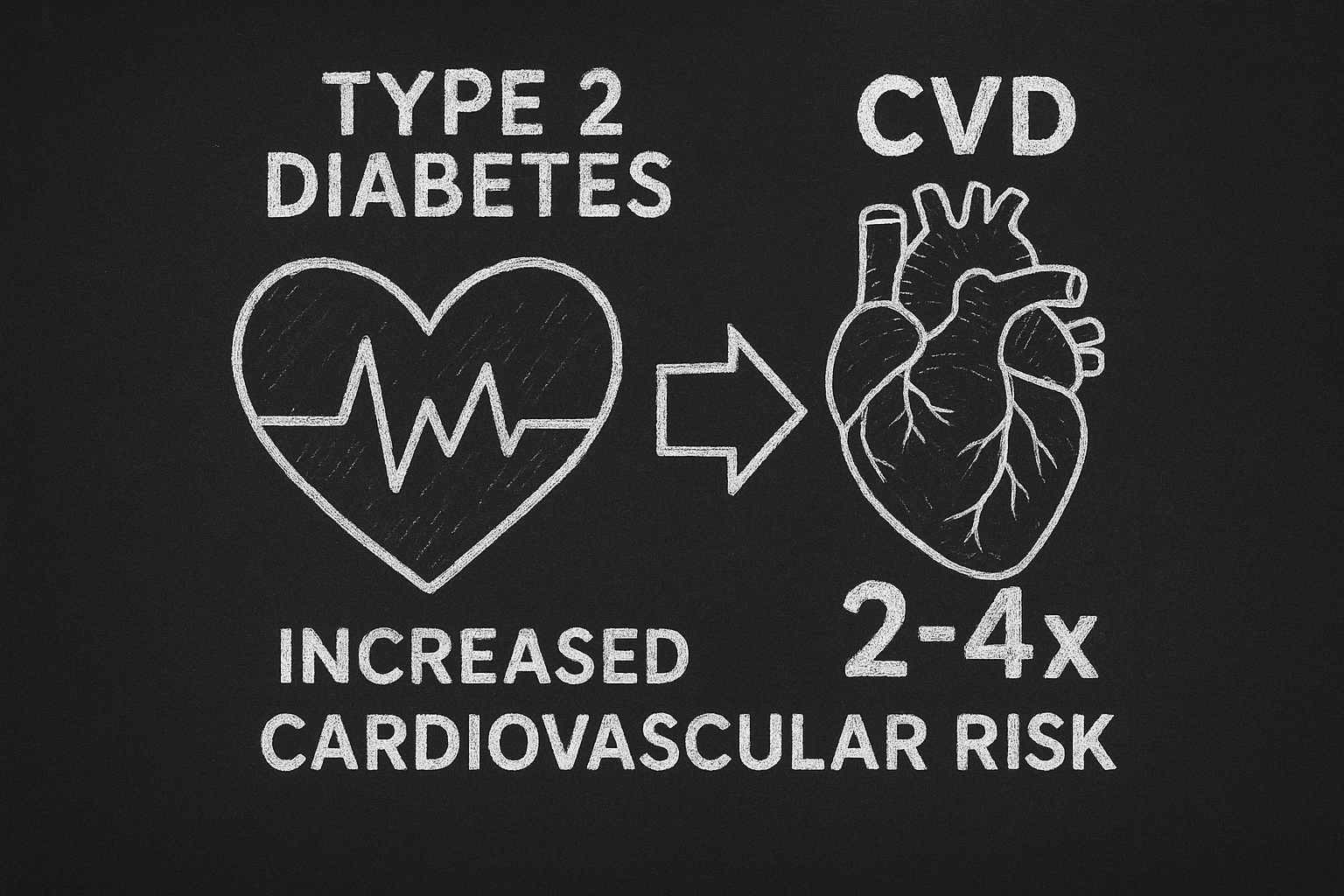
Despite nationwide improvements in cardiovascular disease (CVD) mortality and morbidity, deaths among adults with Type 2 diabetes are two to four times higher than those without the disease. A key contributor to these outcomes is patients not taking their medication as recommended.
Taking care of her brother when he lost his leg to diabetes is what finally prompted Jane to see her doctor. She was shocked to see her A1c at 11.6%.
“I needed someone to scare me. No one was doing that until I saw that A1c. Once I saw that, I was ready for the program.”
 Last year, Jane enrolled in Office-Guideline Applied to Practice (Office-GAP) IMPACT, a program designed to improve medication adherence and prevent cardiovascular disease in patients with diabetes. With funding from the National Institutes of Health (NIH), Adesuwa "Ade" Olomu, MD, MS, associate dean for faculty affairs and the Blanch B. & Frederick C. Swartz Endowed Professor of Medicine at the Michigan State University College of Human Medicine, and her co-investigators are studying how the program can help patients take control of their health.
Last year, Jane enrolled in Office-Guideline Applied to Practice (Office-GAP) IMPACT, a program designed to improve medication adherence and prevent cardiovascular disease in patients with diabetes. With funding from the National Institutes of Health (NIH), Adesuwa "Ade" Olomu, MD, MS, associate dean for faculty affairs and the Blanch B. & Frederick C. Swartz Endowed Professor of Medicine at the Michigan State University College of Human Medicine, and her co-investigators are studying how the program can help patients take control of their health.
Olomu’s Office-GAP IMPACT program takes place in Federally Qualified Health Centers (FQHCs) in three counties in Michigan with the help of clinical research coordinators like Sandy Samp. She met Jane at Alcona Health Center in Alpena County.
“Half the battle was meeting Sandy,” said Jane. “What a peach. We’re just so much alike.”
Sandy and Jane’s relationship bloomed through the Office-GAP IMPACT program, which helps patients and providers work together. The program provides an initial educational group visit and simple checklists that are completed jointly by the patient and provider during regular office visits. Patients are followed during office visits for one year at one month, three, six, nine, and twelve months.
“I just love connecting these individuals with the resources needed to help them understand diabetes, in turn helping the participants truly get what they needed to make it easier to self-manage their health,” said Sandy.
The Office-GAP IMPACT program consists of several steps created to educate and support the patient. First, patients learn the medical evidence behind their diagnosis and treatment and how to become active in their self-care. Second, patients and providers partner together using a checklist to guide conversations and decisions.
“What’s cool about the program is that we are providing tools and building communication skills to help people do what they already have within themselves to do – to partner with their providers to make the best decisions they can about their health, said Karen Kelly-Blake, PhD, associate director in the Center for Bioethics and Social Justice and co-investigator of the study. “Doing that piece, and doing it well, is a game changer.”
“I started doing things and I was feeling better about myself. The first time I went (back to the clinic), I was down to an A1c of 8,” said Jane.
A third step of the program is Way2Health, which consists of text-based health messages, tips, and reminders. Texts reading “Would you eat peanut butter and celery, nuts, carrots or an apple instead of chips or cookies if you had them ready? Planning ahead makes snacking healthier” and “Making a grocery list can keep you on track at the grocery store” are sent to patients one to three times a day.
“The educational modules cover a range, but the messages are, typically, reminders to do self-check-ins with blood pressure, food choices, and glucose monitoring,” said Dr. Kelly-Blake. “Several participants have shared that the messages were a source of encouragement and accountability to stay on track.”
“Building trusting relationships with everyone on the team including the participants, made the year with these ladies seem like it went by so fast,” said Sandy. “I couldn't wait to see what their A1c was going to be, because I knew they wanted to get better. I feel meeting each one where they are in their journey and speaking on their level of understanding really helped build relationships throughout the year.”
After a year of the program, Jane was well on the path of taking control of her diabetes with information and healthy habits.
 “This program helped me. It educated me. It made me understand the seriousness of this disease. It made me see, more importantly, that I can change this. I was in control; it wasn't the diabetes."
“This program helped me. It educated me. It made me understand the seriousness of this disease. It made me see, more importantly, that I can change this. I was in control; it wasn't the diabetes."
Dr. Olomu says testing interventions in FQHCs are critical for achieving health equity. It ensures that innovations in care delivery are informed by and effective for the very communities most affected by disparities—transforming evidence into action where it is needed most.
“The most important aspect of this research is its potential to transform how care is delivered to underserved populations—by producing rigorous, real-world evidence that leads to more equitable, effective, and sustainable health care models,” said Dr. Olomu.
The research continues through April of 2026 in Saginaw, Lansing, and a dozen Alcona Health Center locations.
For Sandy and Jane, the research sparked not only a friendship, but a healthier path forward for both women.
“This research program isn't just a job, it's been a life changing experience I will carry with me forever,” said Sandy.
"Every time I look at one of my grandbabies, I think I'm going to be there for their wedding,” said Jane. "This program would be great for so many people."
Research Rescue Fund![]()
Spartan researchers are dedicated to understanding the world’s most pressing health challenges and improving the health of all people. In these uncertain times, our most important research is at risk. A gift to the Research Rescue Fund can help bridge funding for the groundbreaking work happening at the College of Human Medicine.


