Dean's Update
July 1, 2021 - Aron Sousa, MD
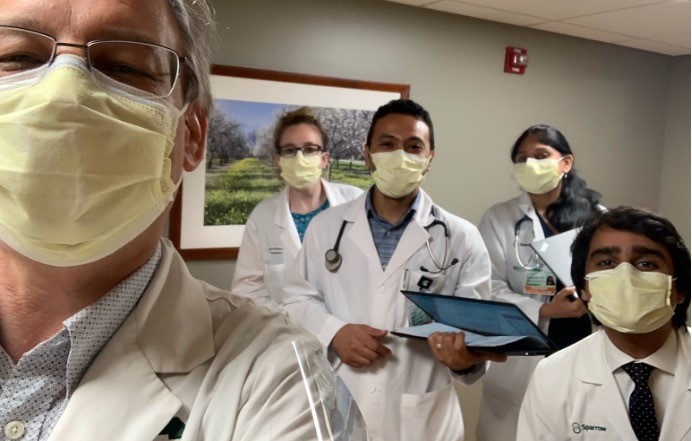
Photo: L-R Me with first-year residents Dayna Dines and Ahmed Maky, and new senior residents Keerthi Gullapalli and Fahad Salam
Friends,
What a difference a few months make. This week I started my fortnight of rounding at the hospital, and my team’s census includes only one patient with COVID-19. When I started rounding in April, half of the patients assigned to the team had or were recovering from COVID-19. It is true that cases were down last July as well, but there are even fewer this year compared to the summer of 2020. That is the power of our vaccines and the dedication of people who have been vaccinated. More on that in a moment.
Rounding on July 1 is different than hospital work any other day of the year. All across the country, July 1 is the first day of the residency calendar. As June 30 turns to July 1, residents are promoted to their next year of training, so fourth-year surgical residents turn into chiefs, interns turn into senior residents, and graduating residents turn into fellows or attending physicians. Even if you are not graduating or being promoted to new responsibilities, the people around you are in new roles.
I am fortunate to be rounding with new first-year residents Dayna Dines and Ahmed Maky, and we are led by new, intrepid senior residents, Keerthi Gullapalli and Fahad Salam. Our medical system depends on residents to provide all manner of high quality, low-cost service to patients and their families. They are also the future of the profession. The general standard is that residents work about 80 hours a week, often with on-call or night shifts that bend their circadian rhythms while working in systems they do not control, but for which patients and attendings often hold them accountable.
That is not a rosy picture, but for most physicians, residency was the best and hardest part of their training. It is easy to imagine that we value those things for which we worked hardest, so the value of residency could feel big because the commitment and effort to succeed in residency is so large. But in my view, residency is genuinely a remarkable educational model. Residents have authentic responsibility for patients – they write real orders and do real procedures that can help or hurt people. Additionally, residents are nearly always surrounded by, and kept out of trouble by, people more expert than they. Sometimes those experts are more senior residents and sometimes they are attending physicians. Authentic experience is a necessary part of curricula that aims to create real world performance. This kind of authentic experience used to be common in the medical school training as well, but billing rules, electronic health records, increased focus on board examinations, and changes in the organization of health care have combined to make creating an authentic clinical experience for students more and more difficult. Our Shared Discovery Curriculum is explicitly designed to provide those authentic clinical experiences so many of us value from residency.
During the COVID-19 pandemic, residents soaked up much of the additional patient load because teaching hospitals added more ICU or emergency department rotations to their schedules. Many of our residents have gone for months working six days a week, 80 hours a week without a vacation. In that sense, residents really did carry many of our teaching hospitals through the pandemic. And residents, like other care providers, will be challenged by this crisis long after the pandemic ends. There is correlation between time treating COVID-19 and mental health struggles in physicians and health workers. We do need to look out for each other.
Hopefully, and if enough of us get vaccinated, we will not see our health system stretched to that point again. The delta variant is the main concern for a meaningful outbreak among the unvaccinated in the fall…or sooner. The vaccines in the US cover delta, and as I’ve said so many times before – and it’s still worth repeating: to protect yourself and those around you, please encourage vaccination.
Serving the people with you,
Aron
Aron Sousa, MD
Interim Dean

