Patiently Gazing into Patients’ Lives
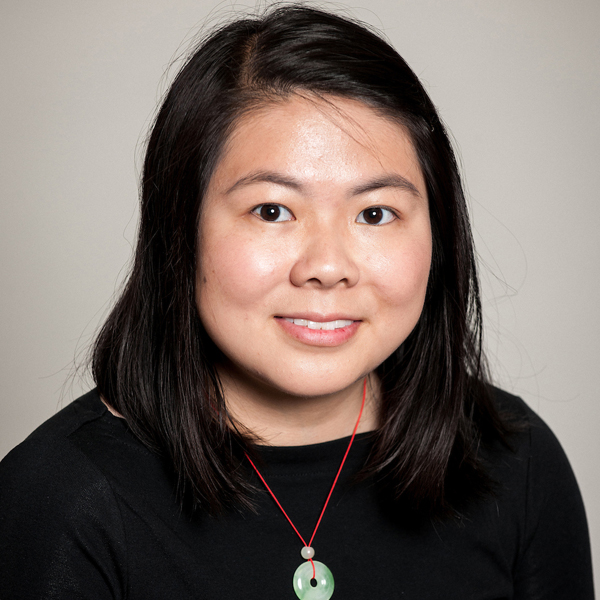
January 1, 2019 - Annie Li Yang
Annie Li Yang was a first-year medical student at the Michigan State University College of Human Medicine. She held a BA from Princeton and would have received her MD in 2022. Annie sadly passed away in late June of 2019.
Below is her winning 2019 Inaugural Student Essay Contest entry titled “Patiently Gazing into Patients’ Lives." The contest has since been named the Annie Li Yang Student Essay Contest.
When I was on the cusp of matriculating at the College of Human Medicine a few months ago, I grappled with a nagging fear. Not fear of entering the field of medicine, but fear that the deeper I delved into the basic and social sciences in medical school, the more I would be led to reduce a patient to a collection of illnesses. I had just started reading Michel Foucault's treatise, The Birth of the Clinic, which stresses the concept of the medical gaze as a reduction of a patient to bodily ailments. Would I lose sight of the patients' lives and identities in the process of learning about the pathophysiology or pharmacology? To my relief, my experiences in the Shared Discovery Curriculum have been anything but reductive.
 During our first week as medical students, Dean Beauchamp reminded us that patients "won't care about how much you know, until they know about how much you care." The significance of this aphorism was not fully impressed upon me until Clinical Simulation Lab began, and I emerged from a trial by fire: the first round of recorded patient interviews. I distinctly remember my heart sinking while watching my own video during Post Clinic Group – watching my inept attempts to address the simulated patient's emotions. When the patient expressed fears about missing work, I briefly touched upon his concerns and then launched into questions about his illness. I had treated him like nothing more than a constellation of symptoms.
During our first week as medical students, Dean Beauchamp reminded us that patients "won't care about how much you know, until they know about how much you care." The significance of this aphorism was not fully impressed upon me until Clinical Simulation Lab began, and I emerged from a trial by fire: the first round of recorded patient interviews. I distinctly remember my heart sinking while watching my own video during Post Clinic Group – watching my inept attempts to address the simulated patient's emotions. When the patient expressed fears about missing work, I briefly touched upon his concerns and then launched into questions about his illness. I had treated him like nothing more than a constellation of symptoms.
I blamed, in part, my training in journalism that had left me with the yearning desire to piece the symptoms together into a disease. But, my classmates had experienced the same inner conflict. Indeed, it was much easier to launch into questions about the duration of the patient's fever than it was to untangle complex emotions that transcended the office. It was much easier to ignore social determinants of health, simply because they are difficult to change in a single office visit. Fortunately, the nature of the Shared Discovery Curriculum ensured repeated simulated patient encounters, which eventually dismantled our fears. It was much more difficult to address patients' emotions and backgrounds, but we knew that it was right. While societal inequalities are difficult to address, they are crucial in providing quality, patient-centered care.
My ability to address social determinants of health was put to the test when I entered my early clinical experience at the MSU Family Health Center. One of the first patients I roomed was not unlike my grandmother in that she spoke Mandarin Chinese and had that same independent spirit. Although she spoke English well, I could tell that it was difficult for her to convey all her concerns to the medical assistant, as many were lost in translation. Filling out the paperwork for her annual wellness exam was similarly difficult. Taking Dean Beauchamp's words to heart, I offered to go over the forms with her while we waited for the physician to arrive; watching her eyes light up when she found out that I also spoke her mother tongue was unforgettable. From my brief interview, I was able to not only learn more about her family history but also unearth an urgent health concern. I was asked to remain in the exam room as an interpreter, and afterwards, the patient expressed her gratitude for conveying her concerns, many of which she believed were embarrassing, to the physician on her behalf.
Over the course of these intervening weeks, I've come to realize that I'm one of the few people privileged to see patients at their most vulnerable. For many of the patients, coming to the office and talking about their pains, both emotional and physical, is a deeply difficult act. Seeing patients become vulnerable has always struck me with the immense trust patients have in those taking care of them. As such, these clinical encounters have lent new meaning to "patientcentered interactions." So instead of launching into preferred pharmacies and vaccination histories, I take a few moments to express genuine interest in their lives for those few minutes, ask about their six dogs and cats, if they had any trouble getting into the office. When I open up, offer patients a chance to talk about their lives, they open up too.
And I've felt so privileged. Privileged to see their travels, their tattoos, their wounds. It's difficult to put into words the smile that crosses the patient's face when I ask about their vacation, and even more difficult to put into words the smile that crosses mine when they pull out their phones and show me. When I encounter patients at the grocery store and they give me a wave, I finally understand what it truly means to become a physician. To see the patient as someone much like myself, a member of a wider community and family.
The Shared Discovery Curriculum, with its emphasis on collaboration and clinical experiences, has undoubtedly allowed me and my classmates to improve our clinical skills. At the same time, the basic and social sciences offered through Large Group Activities, Virtual Imaging & Physiology Lab, and Gross Anatomy Lab are indispensable in understanding the whole body on macroscopic and microscopic levels. Balancing these aspects of medicine has lent greater meaning to our medical school education and patient encounters.
Although I write with the gaze of a first year, Early Clinical Experience student, I feel that my peers and I have matured beyond our years. It's amazing how fearless we've become with only one semester in the books, unafraid to tackle patients' fears and complex emotions head on. When we enter the Middle and Late Clinical Experiences, we'll know how to NURS and interact with health care teams. When we face difficult moments, we'll know how to support one another and share discoveries. And I know that when my peers and I graduate from the Shared Discovery Curriculum, we'll lend new meaning to the phrase, "I'm part of the medical team taking care of you today."

